Pelvimetry
A huge surprise for me in my midwifery education? The pelvis, and my sudden and unequivocal love for it. Second big surprise? That you can measure the pelvic bones through the vagina. Fancy term for that? Pelvimetry. Mind = blown.For those involved with birth, the pelvis holds great interest, promise and beauty. A mix of generally static bone structure, flexible cartilage, and stretchable ligaments, the pelvis is in the position of the woman controlling it, and is the passage to be navigated by the baby maneuvering its exit. With any bimanual examination, during which the provider is assessing the cervix, uterus, ovaries, or vaginal tone, they also may indirectly measure parts of your pelvis. Did you know? Has anyone ever informed you that they are checking your pelvic bones through your vaginal muscle? Have you ever wondered how someone knows that a baby could fit through your pelvis? Do you think that just because you wear a smaller pant size that your pelvis might be too small for birth?Midwives and obstetricians are taught the art of pelvimetry, or pelvic measurement. How do I know this? Because it is outlined in both of our key educational resources: Varney's Midwifery and Williams Obstetrics. And because I was taught how to do it. And because I know midwives who measure pelves regularly, and I overhear obstetricians talking about it. It is on people's minds in obstetrics, and I think few women know about it. So, let's start with a quick video. Her explanation of pelvimetry is far, far better than the education I received in midwifery school, and far better than what I could type up here regarding the step-wise approach.Generally, resources reference four types of pelvises / pelves: gynecoid, android, platypelloid, and anthropoid. The gynecoid pelvis is generally thought to be the most common type. The top picture following this paragraph is of a gynecoid pelvis and anticipated measurements, and followed by pictures of the posterior (p) and anterior (a) changes in the other pelvic types. Generally, we are looking for a wide transverse inlet for engagement, roomy diagonal/obstetrical conjugate for descent, and forgiving interspinous diameter for exit.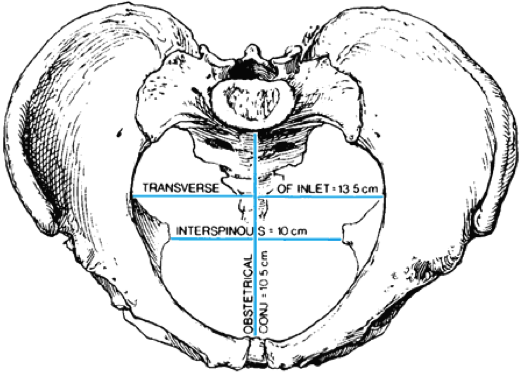
 Note: These pictures were provided through a student file share, and found incidentally in Williams Obstetrics while during research for this post.Aren't they beautiful?!? What is there to love about the pelvis? Its size, shape, diversity, and flexibility. The inlet, the outlet, spines, curvature, and prominences. Perhaps I digress, or I have only just begun. Important to note for those new to pelvic anatomy is that the final parts of the spine and coccyx are flexible and move out of the way during birth, while the spines on the left and right stay right where they are. However, the bones to which the spines connect are connected by joints and ligaments, and are thus flexible. A wild world, right!?What is happening in the above pictures, and what are providers looking for? Variations on all four types are possible, and mix and matches of each type can be found in each pelvic arrangement. We hope for a roomy pelvis that has mostly gynecoid features, again with the largest image above. Why? If you think about a round-ish baby's head engaging in the pelvis, naturally it may tend toward certain positions given certain bony structures. Some believe that certain pelvic types:
Note: These pictures were provided through a student file share, and found incidentally in Williams Obstetrics while during research for this post.Aren't they beautiful?!? What is there to love about the pelvis? Its size, shape, diversity, and flexibility. The inlet, the outlet, spines, curvature, and prominences. Perhaps I digress, or I have only just begun. Important to note for those new to pelvic anatomy is that the final parts of the spine and coccyx are flexible and move out of the way during birth, while the spines on the left and right stay right where they are. However, the bones to which the spines connect are connected by joints and ligaments, and are thus flexible. A wild world, right!?What is happening in the above pictures, and what are providers looking for? Variations on all four types are possible, and mix and matches of each type can be found in each pelvic arrangement. We hope for a roomy pelvis that has mostly gynecoid features, again with the largest image above. Why? If you think about a round-ish baby's head engaging in the pelvis, naturally it may tend toward certain positions given certain bony structures. Some believe that certain pelvic types:
- may cause an increased likelihood for fetal head positions in labor, such as transverse or posterior presentations, that can be more difficult to birth;
- ease the process of vaginal birth, with a roomy pelvis leaving no concern for bony obstruction; or
- possibly predict significant problems for an obstructed birth.
Still learning pelvimetry? I vote Heart & Hands by Elizabeth Davis as the best book-resource around, or at least around my own personal library. The drawings are incredibly visually literate for any reader, with overlays of vaginal tissue and underlying bone structure. They just make sense, and for something that is mostly learned by feel, making sense beforehand is incredibly important. Pelvimetry is discussed on only a few pages of the book, but a few pages that are wonderfully explanatory in both words and images.Let's review what this means for midwives and obstetricians, with author by both alphabetical order and, coincidentally, by coolest profession:
- Varney's Midwifery: With a stepwise procedure and rationale in parallel with the description of findings, any provider can easily learn the process of pelvimetry. Varney and authors of this section do allude to the assessment of the findings of pelvimetry as important in relation to the estimated fetal weight (EFW), and specific findings that could cause difficulty at certain points in labor.
- Williams Obstetrics: Reviewing research from 1937-1987, Williams Obstetrics (copyright 2010) could make anyone fearful that their pelvis is in some way contracted or faulty or at risk of completely ruining the possibility of vaginal delivery. There is little rationale or current research related to the utility of pelvimetry at this point in obstetrical care.
And what of the super-scientific crew? Let's start with Oxorn-Foote's Human Labor & Birth, the optimum resource for the human pelvis and birth processes. And, when it comes to pelvimetry, let's finish, because it is a classic but as such is totally out-of-date on multiple things: ranges of measurement, rectal exams of the cervix, and ability to remember anything you have read by the end of the section. Additionally, there is no statement of rationale for measuring a pelvis, just the automatic jump in of the measurements themselves, and what birth may look like with each of the four pelvic types. For learning the bony pelvis and the fetal skull, abnormal presentation and birth ability, as well as cardinal movements and deviations from norm, (also the sweetness on breech deliveries), definitely check this book out. But it's hold on pelvimetry has come and gone. Moving on.Who else advertises pelvimetry in their resources for the obstetric learning community (or at least what is in my library)? Ina May Gaskin in Ina May's Guide to Childbirth (p. 192-193), Elizabeth Davis in Heart & Hands (p. 23-25, 145), and Pam Weaver & Sharon K. Evans in Practical Skills Guide for Midwifery (p. II-46-47). All awesome midwifery resources for checking your personal skill armamentarium.What am I thinking about pelvimetry as of late? There is a specific section in the Electronic Health Record (EHR) of my organization where providers are prompted to complete the clinical pelvic assessment. I have ignored it with each and every patient. I am the first to admit that I rarely measure a woman's pelvis. For women who have given birth before, I do comment about the weight of their prior babies in the initial OB history. I also comment about whether the father of the current baby is the same as prior babies, because I have seen a new genetic line have an impact on fetal size as compared to prior babies. But, those pelvic measurements typically mean very little to me. Additionally, I would not want my record of an abnormal pelvic assessment to allow space for another provider to judge the woman's ability to give birth. And, in the setting where I work, there are some providers looking for any argument against a vaginal birth for some women. I am so fortunate to have been with women on multiple continents as they gave birth to small, medium, and impressively large babies without difficulty. I also attended one woman in my current setting as she gave birth to a small baby with extreme difficulty, from head to hips, a "tight fit" with the mother's anatomy. Was the labor obstructed? No, but it was my first understanding of a "tight fit" not related to the birth of shoulders. So, how does this add up?Let's start with books that I think are important that do not advertise pelvimetry: Penny Simkin's The Labor Progress Handbook; Susan Klein, Suellen Miller, and Fiona Thomson's A Book for Midwives; and Hesperian Foundation's Where Women Have No Doctor by authors A. August Burns, Ronnie Lovich, Jane Maxwell, and Katharine Shapiro. With both Varney's and Williams, I question the general application of this manual skill for women's ability to accomodate a baby's typical navigation pattern. After reviewing Varney's I have a feeling of "Ladies, be warned, your pelvis is potentially adequate as long as your baby's estimated weight late in pregnancy stays within certain parameters." After reviewing Williams, I have a feeling of "Ladies, be warned, your pelvis is potentially a frightening place with every twist and turn according to the fifty years of research ending 25 years ago that we have broadly reviewed and not remotely critiqued." There is no broad statement that inherently every woman's pelvis is a beautiful place for a baby to pass through, and rarely are there variations on that theme.Is pelvimetry a now-being-lost art of obstetrical care, an art that should rightfully be lost? Was its origination largely from the X-ray pelvic measurements for averages that are no longer performed? Is the clinical test of pelvic adequacy through 'proving a birth is possible up to a certain weight' now the baby and the woman showing us that pelvimetry is a bunch of goofy people measuring their hands? Is that a dangerous language path to start on, with "trial of labor until proven inadequate"? Is pelvimetry really most important in situations where an obstetric history is concerning or access to emergency services may be limited? Where is the midwifery, the starting from the place of normal, in pelvimetry?Midwives with whom I have worked have a wide range of opinions about the utility of measuring a woman's pelvis. Some believe that the only true test of the pelvis is birth itself, with clinical notes indicating assurance up to a certain weight, such as 'pelvis tested to 9lbs 3oz.' Some believe pelvimetry is a bunch of malarkey. Some believe it can be a predictor of fetal position, and knowing beforehand allows focusing on certain exercises to encourage best presentation in birth. The most midwife-y answer I have heard to justify its use? Some believe that measuring the pelvis on the first visit helps a woman understand that already her pelvis has plenty of room for a baby, and allows the provider to emphasize that the pelvis only expands during the pregnancy. This is a teachable moment, an opportunity for midwives to assuage fears, and educate on a topic about which woman may have been misinformed.What does the research say? Does pelvimetry really matter for birth outcomes? Up-to-date and The Cochrane Collaboration both summarize the idea of pelvimetry as inadequate in its application to a woman's capability of accommodating a vaginal birth, and name it as not predictive in anticipating a problem with an obstructed labor. Both of these resources are first go-to's for many in clinical practice and in initial research work. Not one shed of research since 2000 has validated that pelvimetry is an important tool for providers to assess pelvic adequacy and anticipate possible labor dystocia or obstruction. And I really looked. I found a few that discuss pelvimetry prior to vaginal breech birth, attempts at vaginal birth after cesarean for prior obstructed labor, and the relationship between height and pelvic diameter in certain African countries where access to higher-level care may be difficult. There are some resources that advertise the flexibility of the pelvis in different positions or debunk the use of clinical pelvimetry (I ignored all those that referred to X-Ray and CT scan):
- Coolest freely available paper I found: Blackadar, C.S. & Viera, A.J. (2004). A Retrospective Review of Performance and Utility of Routine Clinical Pelvimetry, in Fam Med.: "Conclusion: Our study indicates that clinical pelvimetry does not change management of pregnant patients. Current practice is to allow all women a trial of labor regardless of pelvimetry results. This makes the routine performance and recording of pelvimetry a waste of time, a potential liability, and an unnecessary discomfort for patients." Read the full article here.
- Michel, S.C.A et al. (2002). MR Obstetric Pelvimetry: Effect of Birthing Position on Pelvic Bony Dimensions, in AJR: "Conclusion: An upright birthing position significantly expands female pelvic bony dimensions, suggesting facilitation of labor and delivery."
Again, no research was found to say: absolutely, yes, always pelvimetry and here's why. But a lot of interest in the changing pelvic dimension with changing position. Sounds like midwifery to me...What about general labor and birth books, that many people turn to for wisdom and wealth of knowledge, and possibly a little hippie and natural birth foundation? Does pelvimetry hold water?
- Describing the anatomy and physiology of why the pelvis is so flexible: Ina May Gaskin in Ina May's Guide to Childbirth: "In fact, [the pelvis] is composed of four separate bones connected with ligaments at the joints. The hormone relaxin loosens these ligaments late in pregnancy, in preparation for birth, making it even easier for them to shift in relation to one another. The pelvis that might be a little small while you are lying on your back becomes significantly larger when you are on your hands and knees." (p. 193)
- Reviewing that the pelvis is not static even throughout pregnancy, so perhaps pelvimetry in early pregnancy is null and void: Elizabeth Davis in Heart & Hands: A Midwife's Guide to Pregnancy and Birth: "And remember that the pelvis will expand as pregnancy progresses."
- In discussing movements in labor and the flexibility of the pelvis and its role in changing fetal position with maternal position change: Penny Simkin and Ruth Ancheta in The Labor Progress Handbook: "Frequent position changes in labor optimize the chance of a 'good fit' between the fetus and maternal pelvis (helping resolve occiput posterior position, asynclitism, and deflexion). Women often describe less pain when the fetus and pelvis are better aligned, an added benefit. Continuous movement (pelvic rocking, swaying, walking) results in continuing changes in the relationship of the pelvic bones to one another and the shape of the pelvis, which may serve to nudge' the fetus into a more favorable position." (p. 22) Note - read this book for all kinds of great reasons, but also because with any determined fetal head position, there is almost always a maternal movement or position to bring the fetus into a favorable alignment. Brilliant!
With such flexibility and change, it seems there is limited room for static measurement, and lots of room for progress in labor.I do not own Anne Frye's Holistic Midwifery series to read what she thinks about pelvimetry as a process and a rationale, but I wish I did as I greatly respect her opinions on all things related to women's health. However, she is quoted in Davis' Heart & Hands, wisely referring to the ligaments and the joints being influenced by the mother's emotional state, with little influence on the pelvic bones themselves. What an important and lovely consideration for us all.We have not in the least broached the topic of position change, the limit of the term "cephalo-pelvic disproportion," the fetal skull, estimated fetal weight, and maternal body type on the bony pelvis. But I hope this has served as a primer for understanding pelvic measurement.The mystery of the pelvis continues for me. I believe pelvimetry is an incredibly interesting assessment, and one that I have used in international settings where the woman I am working with cannot easily attain emergency care. I also believe there is an incredible amount of flexibility to women's strength in labor, their pelvic flexibility, fetal skull overlap and change, and remarkable maneuvers possible with position changes in labor and birth. And if your love of the pelvis continues, you, too, could end your midwifery education and start your midwifery career with this life-long mark: And how does pelvimetry factor into your practice? Are you a regular pelvis-measurer? Do you support routine pelvic measurements as a routine component of initial OB visits? Do you discuss the flexibility of the pelvis with your patients?
And how does pelvimetry factor into your practice? Are you a regular pelvis-measurer? Do you support routine pelvic measurements as a routine component of initial OB visits? Do you discuss the flexibility of the pelvis with your patients?

